Category: Vensana Capital™ Portfolio News
Relievant Medsystems Announces Updated Policy Statement and Guideline for Basivertebral Nerve Ablation from the International Society for the Advancement of Spine Surgery
MINNEAPOLIS – November 8, 2022 – Relievant Medsystems, a company dedicated to transforming the diagnosis and treatment of vertebrogenic pain, a type of chronic low back pain (CLBP), today announced that the International Society for the Advancement of Spine Surgery (ISASS) has published an updated Policy Statement and Literature Review of Intraosseous Basivertebral Nerve (BVN) ablation in the October issue of the International Journal of Spine Surgery.
The ISASS policy recommends intraosseous BVN ablation as the most successful way to address vertebrogenic chronic low back pain. This update follows the September publication of Best Practice Guidelines on the Diagnosis and Treatment of Vertebrogenic Low Back Pain with BVN Ablation from the American Society of Pain and Neuroscience (ASPN) and demonstrates additional society support for BVN ablation. Relievant Medsystems’ minimally invasive Intracept® Procedure is the only FDA-cleared treatment for chronic vertebrogenic low back pain.
“We see the positive impact that the Intracept Procedure has on patients, and expanded society support of BVN ablation further underscores the efficacy of this treatment for chronic vertebrogenic low back pain,” said Tyler Binney, President and CEO of Relievant Medsystems. “These updated guidelines, in addition to our substantial base of clinical evidence, will help to continue driving awareness and adoption of this proven therapy.”
The Intracept Procedure uses targeted radiofrequency energy to stop the BVN from transmitting pain signals to the brain. The procedure is typically performed in an outpatient surgery center and takes approximately one hour. Based on existing data, patients typically experience minimal post-procedure pain and generally quick recovery times. Patients often feel pain relief within two weeks of being treated with the Intracept Procedure.
About Vertebrogenic Pain
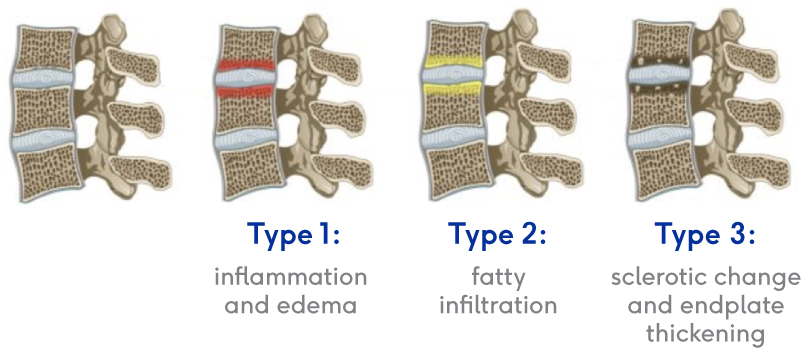
Of the 30 million people in the U.S. with chronic low back pain, 1 in 6 are likely to have vertebrogenic pain, a distinct type of chronic low back pain caused by damage to vertebral endplates, the interface between the disc and the vertebral body. Patients typically have pain in the middle of their low back, which worsens when they bend over, sit for long periods of time, or when they are active. A physician can confirm a patient’s pain is vertebrogenic by observing Modic changes, a biomarker seen on standard MRI that indicates inflammation at the vertebral endplate.
About Relievant Medsystems
Relievant Medsystems is a commercial-stage medical device company transforming the diagnosis and treatment of vertebrogenic pain, a form of Chronic Low Back Pain (CLBP), with the Intracept Procedure – a novel, clinically proven and commercially available treatment designed to improve the quality of life for millions of indicated patients. For more information about Relievant Medsystems and the Intracept Procedure, visit www.relievant.com.
Relievant: Just Clear, Rigorous High-Quality Data
Results from Multiple Clinical Trials Demonstrate the Intracept Procedure is:
Safe
Effective
Durable
Reproducible
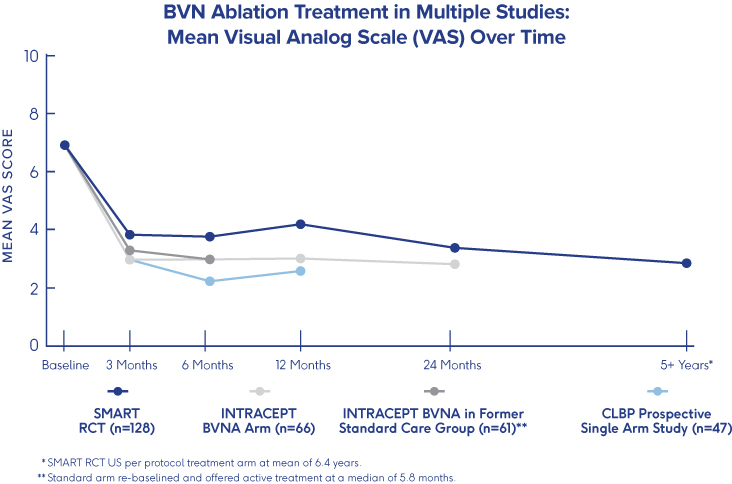
SMART Trial
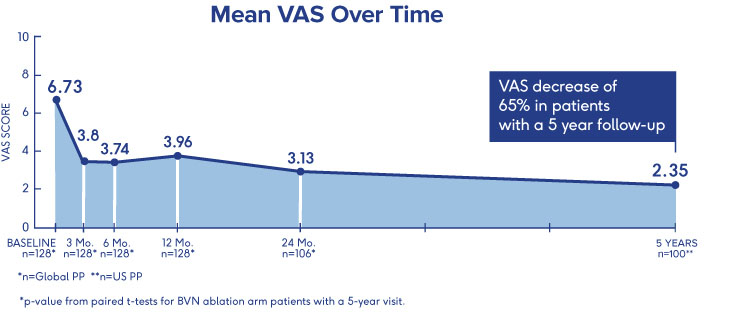
5-Year Durability2
- VAS: 4.38 reduction at 5 years (from 6.74 to 2.35 (p<0.001))†
- ODI: 25.95 reduction at 5 years (from 42.81 to 16.86 (p<0.001))†
- One-third (34%) of patients were pain free at 5 years†
†p-value from paired t-tests for BVN ablation arm patients with a 5-year visit
INTRACEPT Study
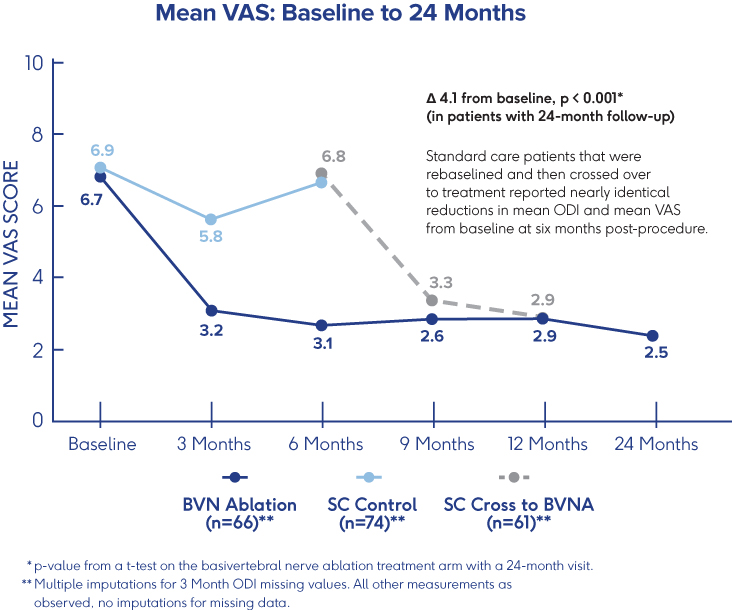
24-Month Results Demonstrate
Sustained Relief 3
- VAS: 4.1 cm mean reduction from baseline to 24 months post-procedure (p<0.001)†
- ODI: 28.5 point mean reduction from baseline to 24 months (p<0.001)†
- 31% of patients were pain-free 24 months after BVN ablation treatment†
†p-values from paired t-tests of BVN ablation arm patients with a 24-month visit
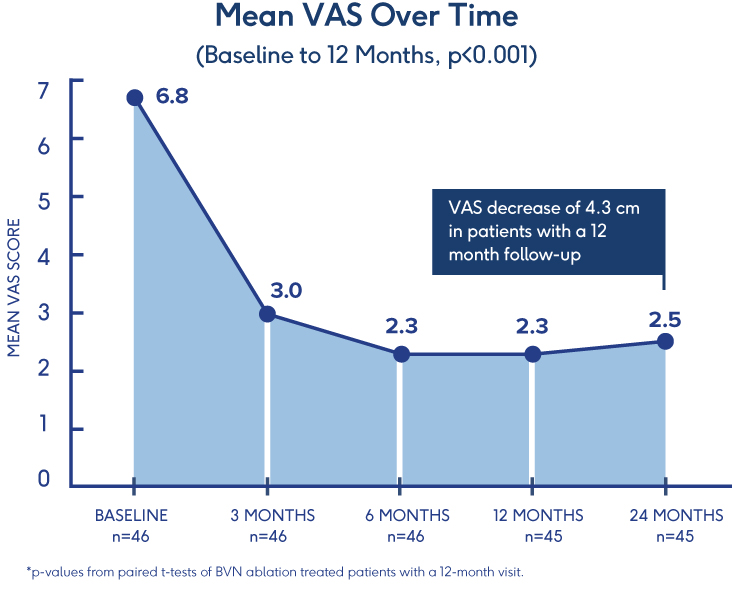
Prospective, Single-Arm Cohort Study
Sustained Relief at 12 Months in
Typical Spine Practices6
- VAS: Mean reduction of 4.3 (p<0.001) from a baseline of 6.82†
- ODI: Mean improvement of 32.31 (p<0.001) from a baseline of 46.98†
- 69% of patients reported >50% reduction in pain while 38% reported being pain-free†
†p-values from paired t-tests of BVN ablation treated patients with a 12-month visit
Pilot Clinical Study
Efficacy of BVN Ablation
in a Clinical Setting 7
- Ablation of the BVN for the treatment of chronic lumbar back pain significantly improved patients’ self-reported outcome early in the follow-up period
- Improvements in function persisted throughout the 1-year study period
- ODI: Statistically significant mean baseline reduction from 52±13 to 23±21 at 3 months follow-up (p<.001); maintained through 12-month follow-up
CLARIFY 2 Affirms Cleerly Over Invasive Heart Disease Evaluation Methods
February 14, 2022
Findings from Cleerly’s groundbreaking echo the recent American College of Cardiology guidelines on the use of CCTA for non-invasive heart disease evaluation.
Instead of proactively identifying patients at risk of heart disease, our industry has historically treated patients once symptoms appear, which can result in late or missed diagnoses, as well as unnecessary referrals to catheterization laboratories.
The CLARIFY 2 study, the second of six studies comparing Cleerly analysis against current gold standards to plaque and coronary artery imaging, demonstrates Cleerly’s effectiveness in the identification and exclusion of high-grade stenosis against traditional core-lab interpreted quantitative coronary angiography (QCA) and invasive fractional flow reserve (FFR) methods. The findings in this study echo the recent American College of Cardiology guidelines on the use of CCTA for non-invasive heart disease evaluation.
AI-Based Evaluation of Coronary Artery Stenosis on Coronary CTA Demonstrated High Accuracy to Core Lab-Interpreted QCA and Invasive FFR
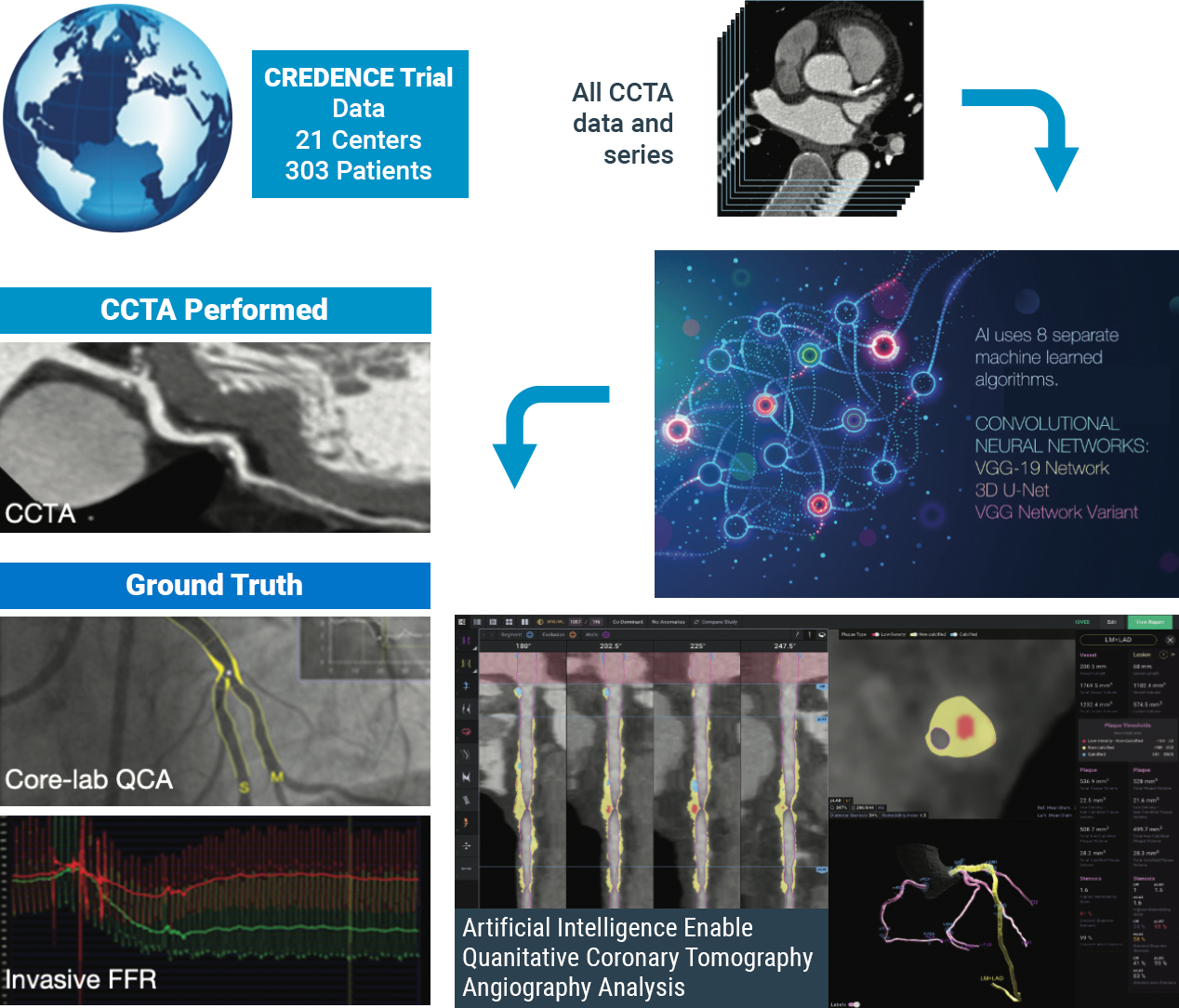
Study highlights include:
Cleerly’s identification and characterization of stenosis is highly accurate (>90% sensitive and highly specific)
Study findings show high diagnostic performance of Cleerly’s non-invasive AI-based evaluation for moderate and severe stenosis at both the ≥50% and ≥70% occlusion levels, along with high correlation to invasive QCA. Importantly, the diagnostic performance of Cleerly’s analysis is similar to results in prior multicenter clinical trials being referred for ACC guideline-indicated invasive coronary angiography.
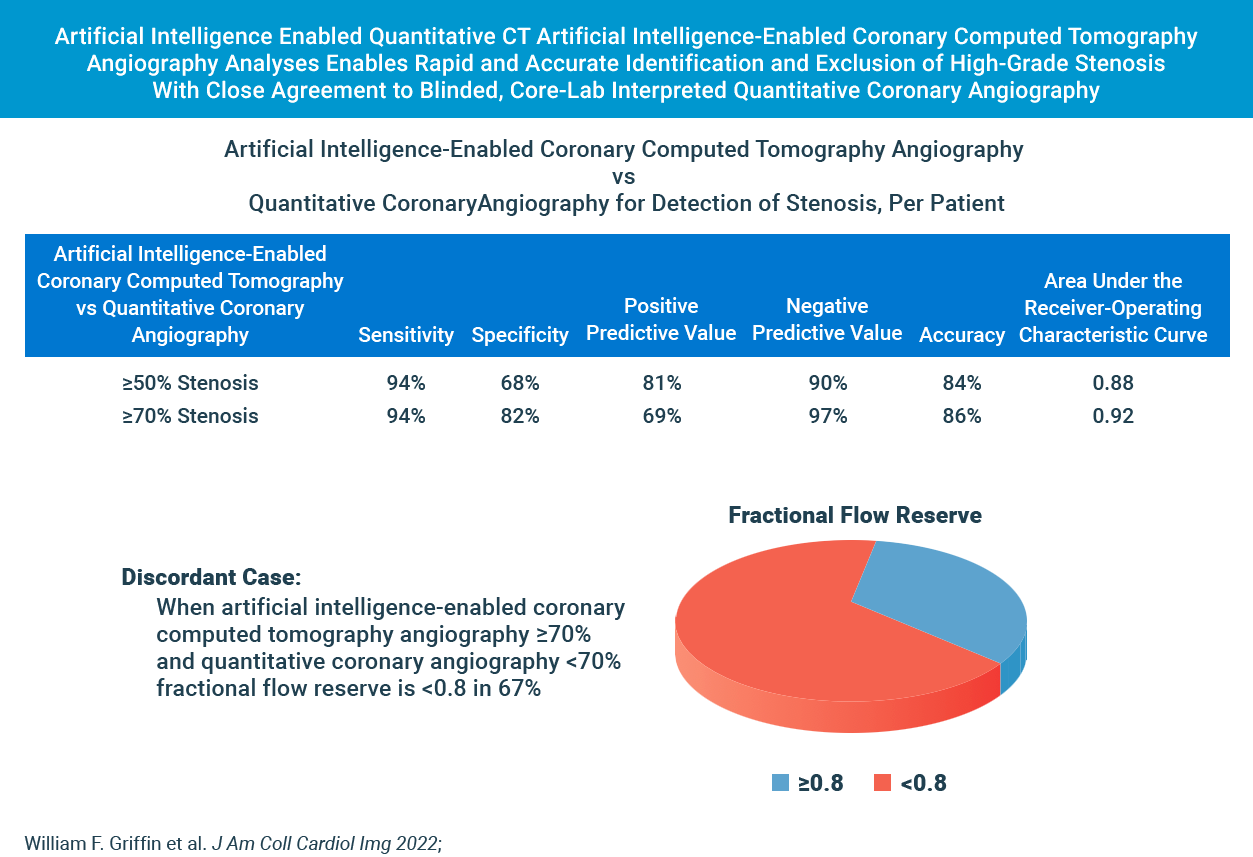
cleerly’s diagnostic performance for moderate and severe stenosis is strong
Cleerly’s AI-based evaluation level of precision is strong based on the area under the receiver-operator characteristic curve (AUC), used to evaluate the diagnostic performance as well as to evaluate the prediction of FFR for both QCA and AI-based CCTA.
The higher the AUC results, the better the model is at distinguishing between patients with disease and no disease. The per-patient AUC is 0.88 for ≥50% moderate stenosis and 0.92 for ≥70% severe stenosis threshold, and a per-vessel AUC of 0.90 for ≥50% moderate stenosis and of 0.95 for ≥70% severe stenosis.
While these scores are numerically higher than those observed by expert core lab readers (AUC: 0.69) and site readers (AUC: 0.57) in the multicenter randomized PROMISE trial, AI-based evaluation for moderate and severe stenosis is significant.
These combined data points offer compelling evidence that clinical use of Cleerly’s AI-based CCTA evaluation serves as an important and useful standard of care for coronary CT interpretation.
| Method | Stenosis | Basis | Sensitivity (95% CI) (%) |
Specificity (95% CI) (%) |
PPV (95% CI) (%) |
NPV (95% CI) (%) |
Accuracy (95% CI) (%) |
AUC (95% CI) (%) |
|---|---|---|---|---|---|---|---|---|
| AI-QCT | ≥50% | Per territory (n = 909) Per patient (n = 303) |
91 (87.1-94.2) 94 (89.8-97.0) |
84 (79.6-86.1) 68 (59.7-75.8) |
69 (64.1-74.4) 81 (74.7-85.5) |
96 (93.8-97.3) 90 (87.2-94.4) |
86 (83.2-88.1) 84 (78.8-87.3) |
0.90 (0.881-0.926) 0.88 (0.843-0.923) |
| QCA | ≥70% | Per territory (n = 909) Per patient (n = 303) |
90 (83.3-94.4) 94 (87.3-97.9) |
91 (88.0-92.8) 82 (76.4-86.8) |
58 (51.0-66.3) 69 (60.5-76.6) |
99 (97.3-99.2) 97 (93.5-99.0) |
91 (88.5-92.8) 86 (81.4-89.3) |
0.95 (0.940-0.966) 0.92 (0.893-0.950) |
| Subgroups based on detection of ≥50% stenosis. AI-QCT = artificial intelligence-enabled computed tomography angiography; AUC = area under the receiver-operating characteristic curve; NPV = negative predictive value; PPV = positive predictive value; QCA = quantitative coronary angiography. |
||||||||
In Cases Where Cleerly and Invasive Angiography Results Disagree, FFR Agrees With Cleerly Over Angiography ⅔ of the Time
The study provides evidence that Cleerly analysis may have performed better than the QCA gold standard used. In the 62 vessels that Cleerly’s estimate of stenosis differed significantly from QCA, we used the “ultimate” gold standard of invasive fractional flow reserve (FFR) to adjudicate the difference. In more than ⅔ of these discordant cases, the FFR result agreed with Cleerly’s output and not QCA.
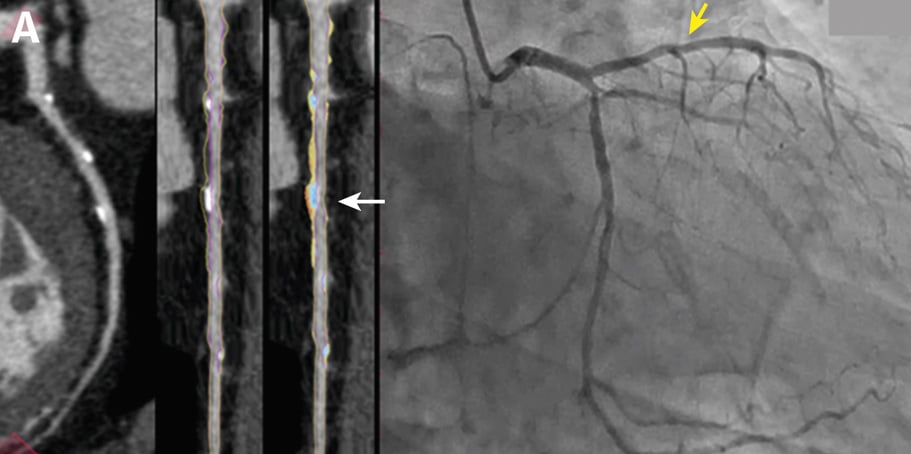
Curved multiplanar reformatted image (MPR) (left), and straightened MPR (second from left) with the lumen boundary (purple line) and outer vessel wall boundary (yellow line) overlay, and with color plaque overlay (second from right) (red is low-density noncalcified plaque [<30 HUs], yellow is noncalcified plaque [31-350 HU], and blue is calcified plaque [>350 HU]). AI depicted a 60% stenosis (white arrow) in the proximal vessel segment. (Right) The left coronary invasive angiogram, in which QCA analysis depicted no stenosis (yellow arrow).
CLARIFY 2 Takeaways
Cleerly’s CLARIFY 2 study aligns with ACC CCTA guidelines and affirms Cleerly’s value over invasive QCA and FFR methods for non-invasive heart disease evaluation. With more than 62% of referrals to catheterization laboratories being unnecessary, cardiac care needs to shift away from treating symptoms and referring patients to the catheterization lab for unnecessary procedures, and focus on preventing heart disease in the first place.
Stay tuned for upcoming results from subsequent CLARIFY studies on the comparison of Cleerly outputs against other gold standards for plaque and coronary artery disease evaluation.
At Cleerly, we focus on identifying patients at risk sooner, quantifying and characterizing disease, enabling personalized and preventive treatment, and improving clinical outcomes that yield significant cost savings for patients and providers.
Envisioning a World Without Heart Attacks: A Call For A New Paradigm of Precision Heart Care
James K. Min, MD, FACC, FESC, MSCCT, Founder & CEO of Cleerly: January 28, 2022
Historically, our diagnostic approaches to patients with suspected heart disease have been restricted to the evaluation of patients with symptoms like chest pain and shortness of breath. Yet, these diagnostic methods fail for the >50% of individuals who will suffer a heart attack without any prior symptoms. This traditional approach misses the majority of heart attack victims for whom heart disease is a “silent killer” that can be prevented through early detection, simple lifestyle changes, and low-cost medical therapy.
Heart disease remains the #1 public health epidemic in the world, causing 1 death every 1.7 seconds. As the leading cause of death and morbidity, heart disease causes more deaths each year than all cancers combined.
Cleerly is a digital healthcare company that is transforming the evaluation of heart disease through precision heart care that measures actual heart disease—atherosclerosis (plaque) that builds up in the walls of the heart arteries—over indirect markers of heart disease, as has been the historical approach. We apply advanced artificial intelligence (AI) technology to non-invasive computed tomography (CT) scans to provide physicians and patients with a heart attack prevention approach that is more personalized and proactive.
Our solutions offer accurate, precise, simple, and rapid heart disease evaluation, with the information delivered to each and every stakeholder in the heart attack prevention care pathway – be they radiologists, primary care physicians, cardiologists, or patients and their caregivers. Through innovative reporting techniques, physicians can now knowingly provide personalized treatment plans and determine whether these treatments are actually halting the progression of heart disease, dramatically improving clinical outcomes, and drastically reducing the costs associated with late-stage cardiovascular care.
Cleerly offers a new and differentiated digital care pathway to prevent heart attacks by delivering the most useful information to physicians and patients in a manner that is simple, stepwise, and logical.
These steps include:
identify and measure actual heart disease, not indirect markers of disease
Historical approaches to evaluating heart disease have relied upon measuring risk factors, such as cholesterol levels in individuals without symptoms; and stress testing in individuals with symptoms to determine whether blood flow is reduced to the heart muscle, a condition known as ischemia. For individuals with symptoms, patients with abnormal stress tests are often referred for invasive coronary angiograms to determine whether a narrowing of the heart artery (referred to as a stenosis) is the cause of ischemia. When considering this diagnostic approach, indirect markers such as risk factors, ischemia and stenosis do not actually measure heart disease, which is the atherosclerosis (plaque) itself.
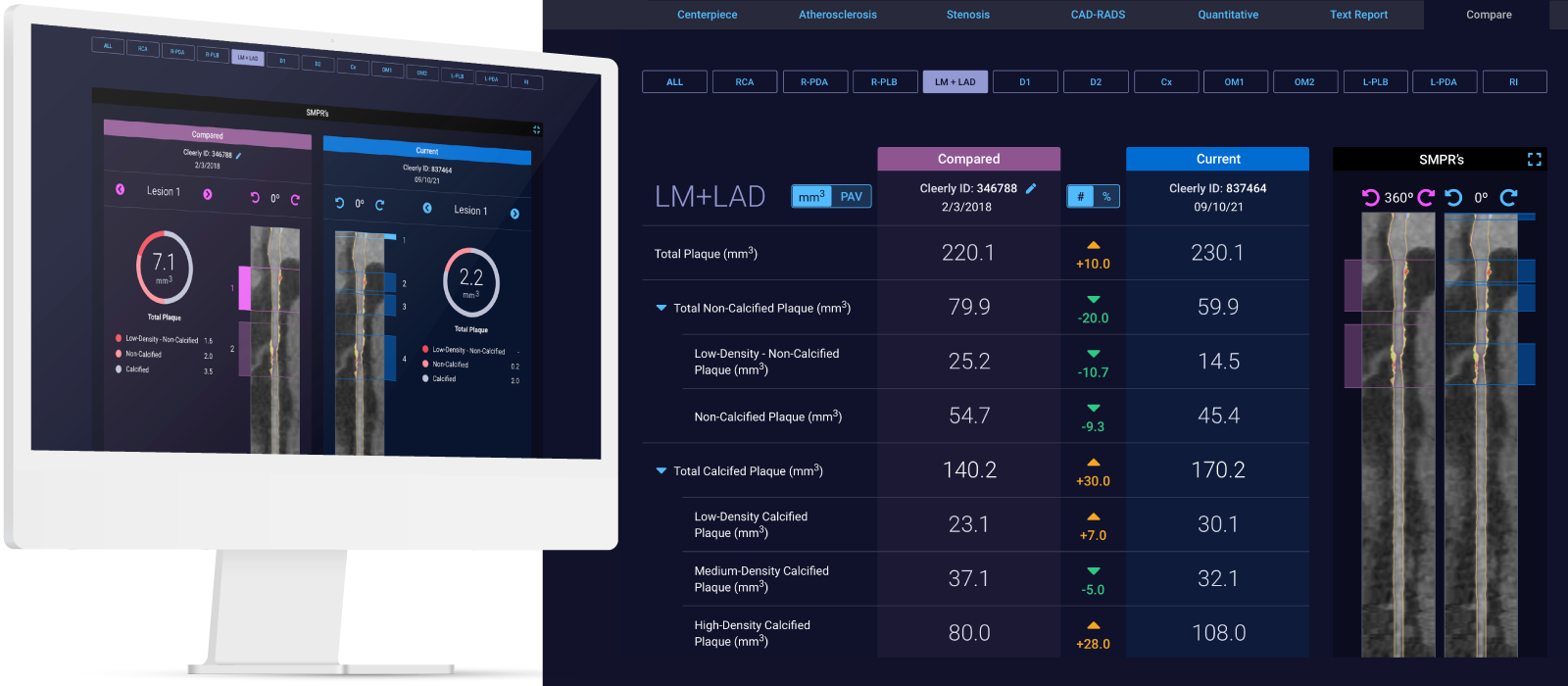
Through research performed over the last 15 years, the field of cardiology has discovered that there is not one but rather many different types of heart disease. Some types of atherosclerosis (plaque) are very dangerous and represent the strongest predictor of which patients will suffer future heart attacks. In contrast, some types of atherosclerosis (plaque) are very stable and, in some cases, can protect against heart attacks. Cleerly’s AI-enabled analyses allow for whole-heart assessment of all of the arteries and their branches for quantification and characterization of the different types of atherosclerosis (plaque) that affect a patient; this allows for a precise understanding of a patient’s heart condition.
Leveraging whole-heart analysis can improve diagnosis and support physicians in their determination of an individual’s risk of heart attack based on atherosclerosis and integration of other contributors of heart disease including genetic, clinical, social, and environmental factors.
translate advanced imaging insights for all healthcare professionals
At Cleerly, we study advanced imaging findings related to heart disease in order to better understand the different types of heart disease, and how treatment with medications and lifestyle affect atherosclerosis (plaque) over time. The improved evaluation of heart disease from advanced imaging is a large step forward towards better understanding heart disease and heart attack prevention.
We recognize that most healthcare professionals are not familiar with advanced non-invasive imaging and may not be aware of the latest research findings. To address this, Cleerly’s digital care pathway translates advanced imaging into actionable clinical insights that can be readily understood and acted upon in real-time by all healthcare professionals, including primary care physicians, nurse practitioners, physicians assistants, general cardiologists, interventional cardiologists, radiologists and many others.

empower patients with knowledge to improve health literacy
After taking care of heart disease patients for two decades, we have observed that patients are much more proactive and involved with improving their health when they actually understand their disease conditions. In this regard, traditional medical reports that we give to patients offer very little guidance in helping them better understand their condition. These reports are too often specialized and require a medical degree to understand.
At Cleerly, we believe that preventing heart attacks requires a team, and the most important member of the team is the patient. While Cleerly’s precision diagnostics are powered by advanced machine learning to deliver precise results on the type and amount of disease present, the results of the Cleerly analysis are provided to patients using web-based interactive tools, personalized reports, and educational resources that help patients make informed decisions about their health.
treat and track disease
Evidence-based, precision medicine for cardiology care is critical for treating actual disease over indirect markers of disease. In this regard, Cleerly has partnered with the American College of Cardiology to emphasize heart disease – atherosclerosis (plaque) – as a primary therapeutic target to encourage physicians to leverage medications and lifestyle interventions that have been proven to reduce the risk of a heart attack.
While our therapeutic “toolbox” for heart attack prevention is heavy—with more than 20 different medications and countless lifestyle changes that are effective at reducing heart attacks—these medications may have different relative benefits in different individuals. In prior studies, the rate of progression of heart disease varies among individuals with rapid progressors of heart disease and those not responding well to medical therapy experiencing the worst prognosis. Cleerly’s technology allows not only for a single evaluation of heart disease, but enables physician tracking of therapeutic success over time to prove that the treatments have halted disease progression and stabilized the atherosclerosis (plaque).
a new paradigm for heart attack prevention
Cleerly’s AI-enabled digital care pathway advances a new paradigm of care that empowers physicians and patients to (1) improve diagnosis, sooner and with greater accuracy and precision; (2) enhance understanding for all stakeholders in the care pathway; (3) guide personalized treatment, whether lifestyle or medical therapy; and (4) track therapeutic success by assessing disease progression and plaque transformation. In doing so, Cleerly’s digital care pathway supports heart attack prevention as the primary goal over more historical approaches where symptom relief is the end goal. We believe that all patients with significant heart disease should be identified early to optimize treatment and prevention. Our AI-enabled digital care pathways model with the translation of advanced imaging science into actionable clinical insights is the first of its kind for evaluating heart disease risk and developing personalized treatment and prevention plans.
While providers have leveraged advanced imaging to encourage personalized medicine to prevent the most common causes of cancer, personalized medicine has not been available for heart attack prevention. Cleerly is making this a reality.
Relievant: When there’s a clear, documented way to diagnose vertebrogenic pain. That’s Living Proof.
The Background
To confirm that a patient has vertebrogenic pain, physicians use MRI to look for specific changes that occur with endplate inflammation, which are called Modic changes.
They’re called “Modic changes” because in 1988, Dr. Michael Modic was the first to publish on identifying and classifying degenerative endplate and marrow changes surrounding a dehydrated intervertebral disc. There were three types of bone marrow changes identified: Types 1, 2 and 3. Types 1 and 2 are the ones that can be used to identify vertebrogenic pain.
Modic Type 1
- Vascular development in the vertebral body
- Findings of inflammation and edema
- NO trabecular damage or marrow changes
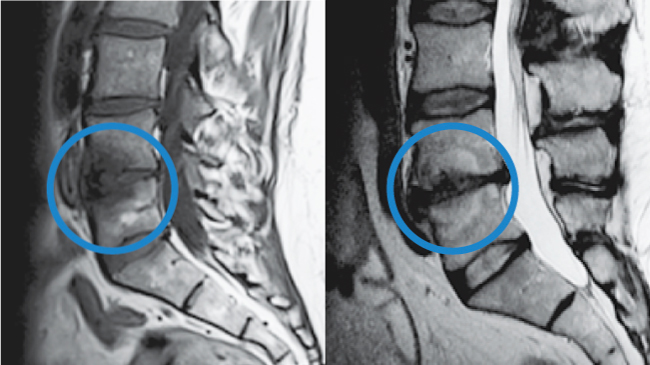
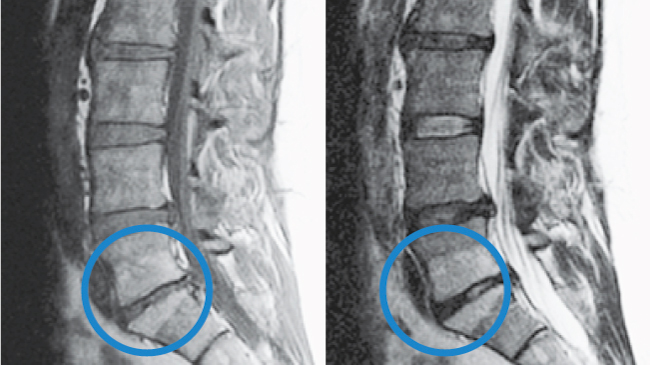
Modic Type 2
- Changes in bone marrow
- Fatty replacement of formally red cellular marrow
- Marrow is substituted with visceral fat
- Same fat located on hips and bellies